Singapore's pandemic strategy
An overview of Singapore’s pandemic strategy.
On this page

What is a pandemic?
A pandemic occurs when a known or novel infectious disease spreads across multiple countries or continents, affecting large populations worldwide. It typically begins as a localised outbreak – characterised by an unexpected increase of cases within a specific area – and may rapidly expand to affect entire regions.
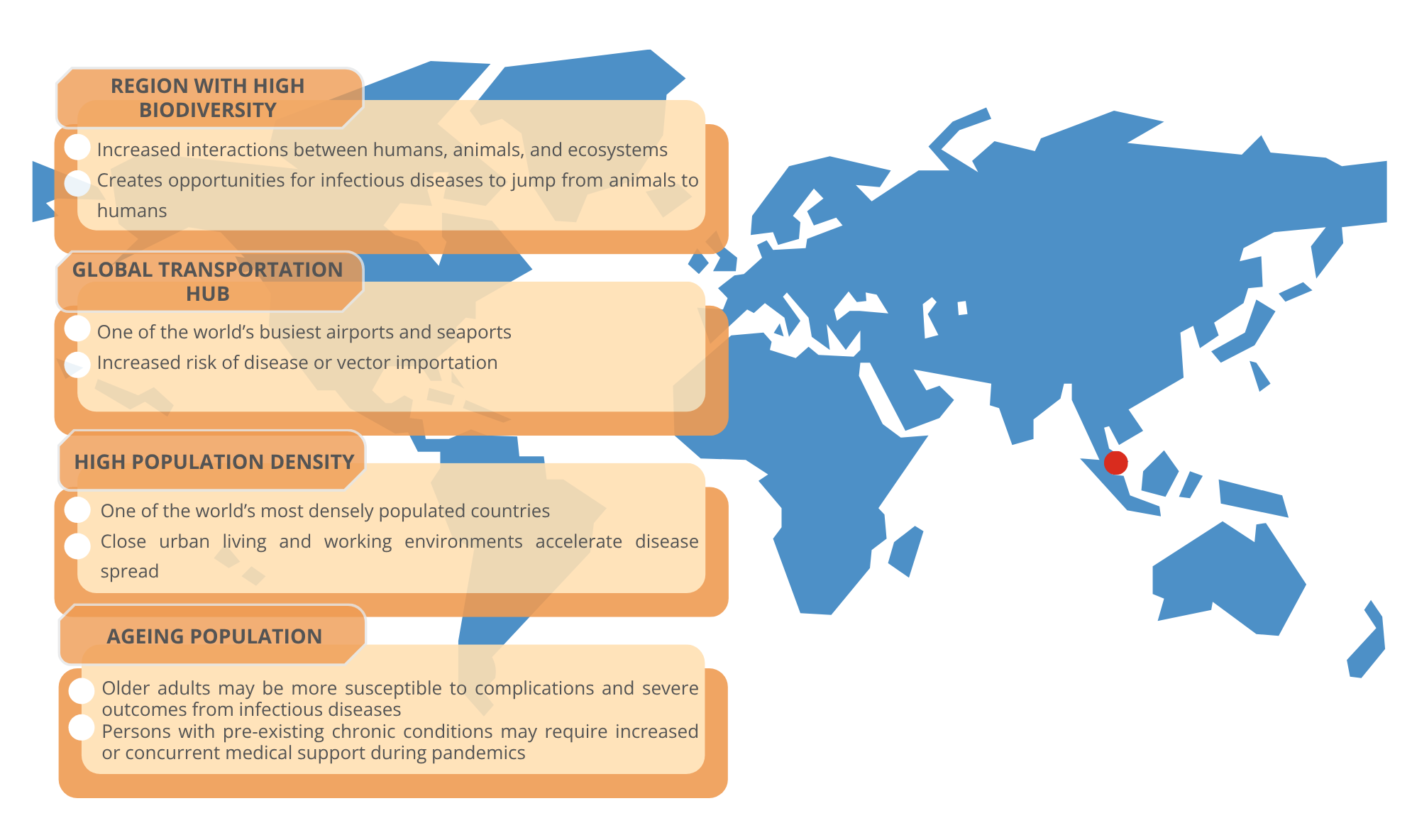
Why is Singapore vulnerable to pandemics?
Singapore is a global trade and travel hub, making it susceptible to the rapid importation of infectious diseases from around the world. We are also located in Southeast Asia, whose rich biodiversity and frequent human-wildlife-livestock interactions makes the region an epicentre for emerging infectious diseases including transmission from animal to humans. Climate change intensifies this threat by altering disease patterns and expanding the range of disease vectors like mosquitoes. Once introduced, the spread of infectious diseases can happen quickly in our highly urbanised environment where people live and work in close proximity. As Singapore’s population ages, there may also be increased healthcare needs during pandemics.
Why is pandemic preparedness important?
Past pandemics, such as COVID-19, have starkly demonstrated how widespread infectious diseases can rapidly disrupt every aspect of life – causing suffering and death, overwhelming healthcare systems, disrupting supply chains, businesses, and education and affecting mental wellbeing. In an interconnected city-state like Singapore, these effects are particularly acute due to our reliance on global trade and travel.
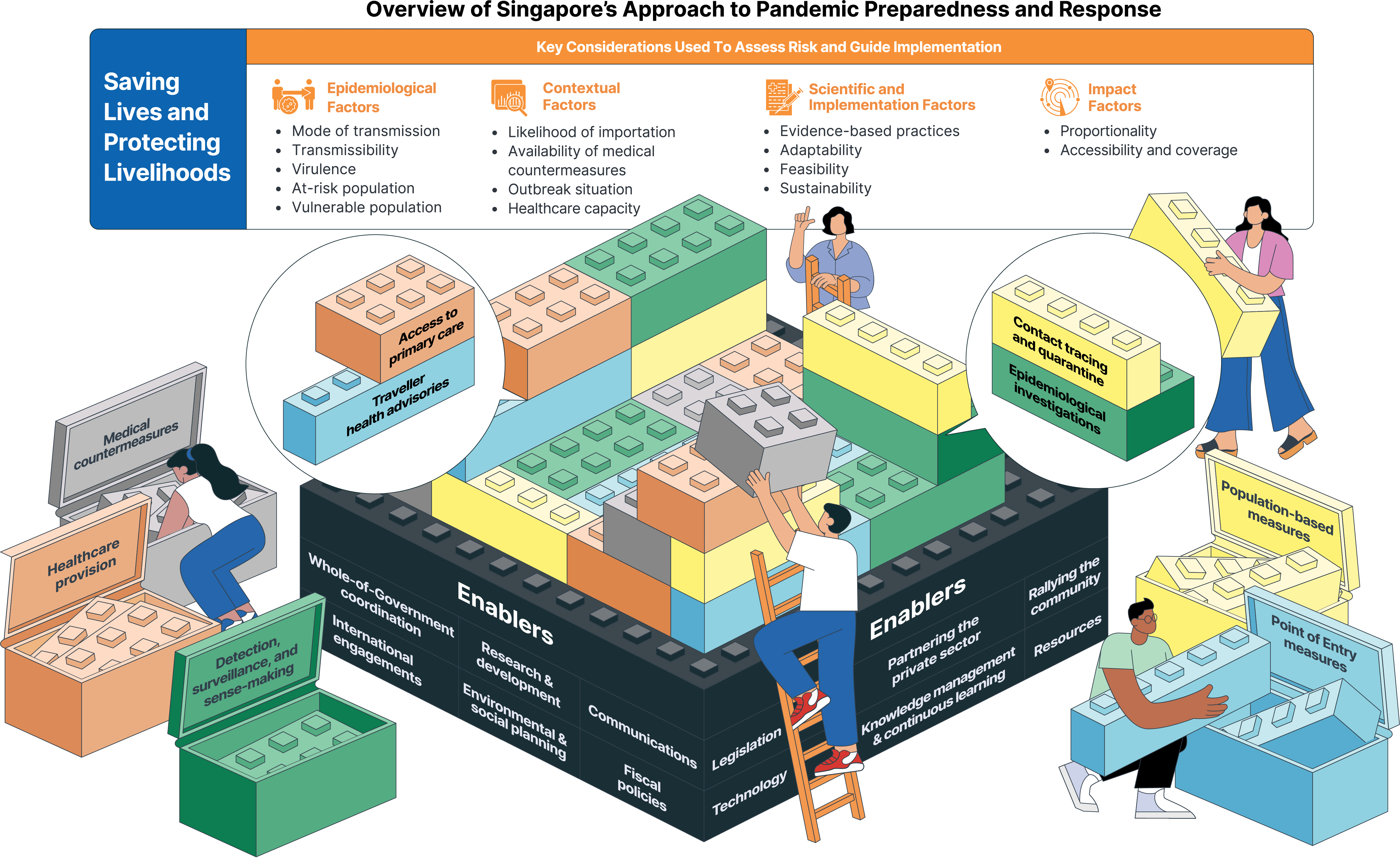
Pandemic preparedness is an ongoing effort and remains a crucial public health priority. Anchored on two overall outcomes – saving lives and protecting livelihoods, these efforts help Singapore maintain critical functions and recover quickly from pandemics.
Singapore Pandemic Preparedness and Response Framework
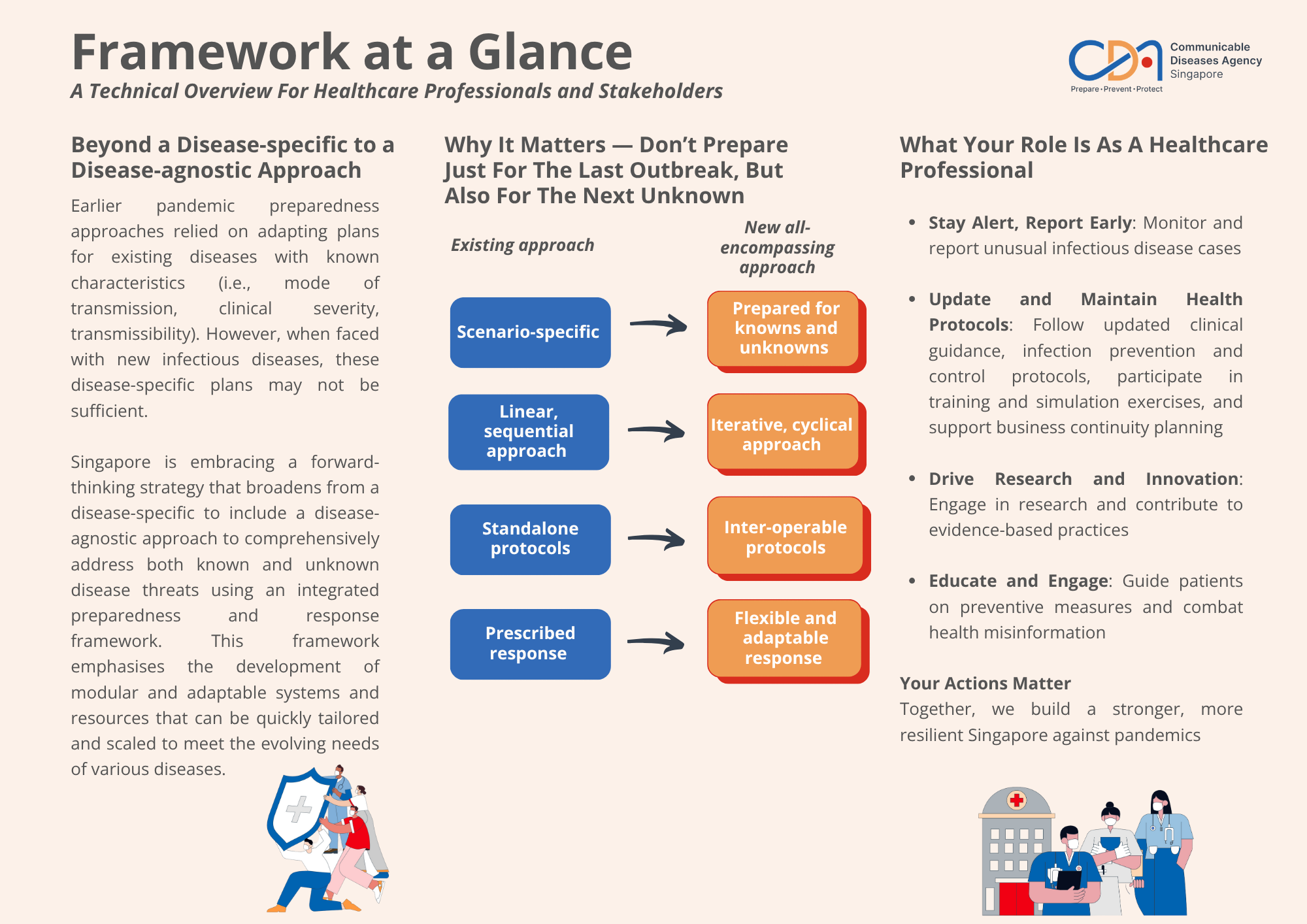
Singapore is embracing a forward-thinking strategy that goes beyond a disease-specific approach to one that is disease-agnostic, acknowledging the unpredictable nature of future health threats.
Launched in 2025, the framework aims to inform our overall preparedness and response efforts, ensuring policies across different sectors are well-informed, coordinated, and aligned with the best practices in public health crisis management. It emphasises adaptable response capabilities that can be rapidly deployed regardless of the nature of the infectious disease threat.
The framework is available here.
What does the framework mean to healthcare professionals?
This framework provides healthcare professionals with insights into national pandemic preparedness strategies and their clinical implications. By understanding how public health responses are developed and implemented, healthcare professionals can anticipate healthcare system adaptations, and effectively communicate these approaches to patients and colleagues.
Healthcare institutions can also use this framework to enhance their emergency preparedness plans, anticipate operational challenges, and develop protocols that ensure continued delivery of essential healthcare services during outbreaks.
The measures
This provides an overview of the measures we can use to manage disease outbreaks, grouped into 5 categories. These categories cover how we detect and monitor infectious disease threats, check and control for diseases at our entry points like airports and seaports, provide healthcare services, deploy medical tools like vaccines and drugs, and implement population-wide measures to slow spread.
These measures can be adjusted based on the disease characteristics and prevailing risk level, ensuring we can respond effectively to different types of disease outbreaks.
.png)
Framework in action
Our framework functions like a sophisticated set of building blocks, which we can add to, remove from, or adjust, as needed. This flexible design enables us to adapt our responses as situations change, while making the best use of available resources.
Drawing upon 4 sets of key considerations, measures across the 5 categories are carefully selected and calibrated, allowing us to create a tailored response to each unique outbreak. There are also enablers that ensure we can implement these measures swiftly and effectively. As we gather more information about an outbreak, we continuously refine our response to safeguard public health and protect livelihoods.
This approach works because stakeholders across all sectors play their distinct roles, from healthcare institutions to business communities and individuals.